Auscultating, or listening to the heart sounds, is a fundamental skill for healthcare professionals. It provides vital information about the condition of the heart and helps in diagnosing various cardiac abnormalities. To effectively auscultate heart sounds, it’s crucial to know where to listen and understand the significance of each auscultation point. In this article, we will explore the key aspects of heart auscultation, including understanding heart sounds, tools for auscultation, the anatomy of the heart and auscultation points, techniques for auscultation, interpreting heart sounds, common challenges, and tips for improving auscultation skills.
Understanding Heart Auscultation
The Basics of Heart Sounds
Heart sounds are the noises generated by the functioning of the human heart. They are produced by the closing of heart valves during the cardiac cycle. The primary sounds heard during auscultation are the first and second heart sounds (S1 and S2). S1 corresponds to the closure of the mitral and tricuspid valves, while S2 coincides with the closure of the aortic and pulmonary valves.
Heart murmurs, which are additional sounds during the cardiac cycle, may indicate abnormalities such as valve malfunctions or structural defects. Identifying and understanding these sounds is crucial in making accurate diagnoses.
Importance of Accurate Heart Auscultation
Accurate heart auscultation plays a vital role in diagnosing and monitoring heart conditions. It helps in assessing heart valve functions, detecting abnormal heart rhythms, and identifying other cardiac abnormalities. By listening to the heart sounds at specific auscultation points, healthcare professionals can gather valuable information about the patient’s cardiac health and make informed decisions regarding treatment.
When performing heart auscultation, healthcare professionals use a stethoscope to listen to the sounds produced by the heart. The stethoscope consists of a chest piece, which is placed on the patient’s chest, and earpieces, which allow the healthcare professional to hear the sounds clearly. The chest piece contains a diaphragm and a bell, each designed to capture different types of sounds.
During auscultation, the healthcare professional carefully moves the stethoscope across different areas of the chest to listen to specific heart sounds. The sounds produced by the heart can vary depending on the position of the patient, the presence of underlying conditions, and other factors. Therefore, it is essential for the healthcare professional to have a thorough understanding of the normal and abnormal heart sounds to accurately interpret what they hear.
In addition to auscultation, other diagnostic tests such as echocardiograms and electrocardiograms may be used to further evaluate the heart’s structure and function. These tests provide detailed images and measurements that can aid in the diagnosis and treatment of various cardiac conditions.
Tools for Heart Auscultation
Stethoscope Selection and Use
The stethoscope is the primary tool used for heart auscultation. Selecting the appropriate stethoscope is essential for obtaining clear and accurate sounds. Different stethoscope models offer varying levels of sound amplification and ambient noise reduction, so it’s important to choose one suited to your needs. Additionally, using the stethoscope correctly, positioning it on the patient’s chest, and adjusting the earpieces properly are crucial for optimal sound transmission.
Advanced Auscultation Devices
Besides traditional stethoscopes, advanced auscultation devices, such as electronic stethoscopes and digital auscultation systems, are gaining popularity. These devices offer enhanced sound amplification, noise cancellation, and the ability to record auscultation findings for further analysis. While traditional stethoscopes remain the gold standard, these advanced devices can be helpful in certain situations, such as in noisy environments or when additional features are necessary.
Electronic stethoscopes, for example, are designed with built-in amplifiers that can significantly enhance the sound quality. This is particularly beneficial when listening to faint heart murmurs or abnormal heart sounds that may be difficult to detect with a traditional stethoscope. The amplification feature allows healthcare professionals to better assess and diagnose cardiac conditions, leading to more accurate treatment plans.
Digital auscultation systems, on the other hand, take auscultation to a whole new level by incorporating advanced technology. These systems consist of a digital stethoscope connected to a computer or mobile device, which allows for real-time visualization of heart sounds. The visual representation of the heart sounds can aid in identifying subtle abnormalities or patterns that may not be easily discernible by listening alone. Furthermore, digital auscultation systems often come with software that enables the recording and storage of auscultation findings, facilitating collaboration and continuity of care.
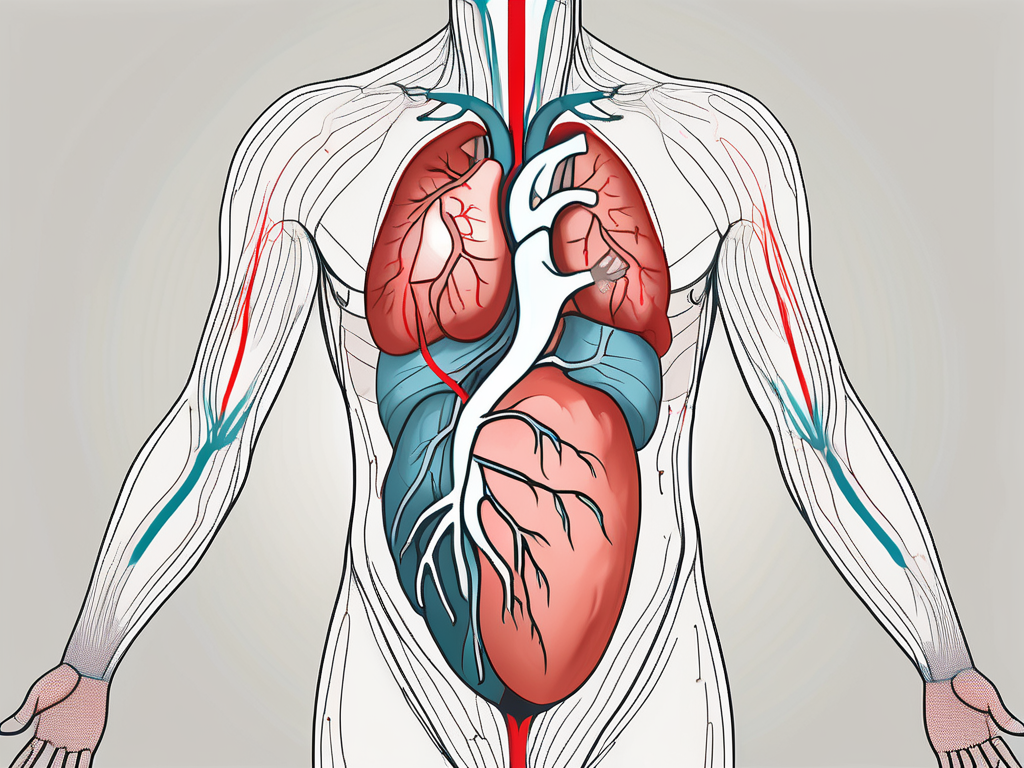
Anatomy of the Heart and Auscultation Points
The Four Heart Valves
The human heart is a remarkable organ that plays a vital role in circulating oxygen-rich blood throughout the body. It consists of four valves, each with its own unique position and function in regulating the flow of blood. These valves are like gatekeepers, allowing blood to flow in one direction while preventing any backward flow.
The first valve we will explore is the mitral valve, located between the left atrium and the left ventricle. It is composed of two flaps, or cusps, that open and close synchronously to ensure the proper flow of blood from the atrium to the ventricle.
The tricuspid valve, on the other hand, is situated between the right atrium and the right ventricle. As its name suggests, it consists of three cusps that work together to prevent the backflow of blood from the ventricle to the atrium.
Moving on to the aortic valve, it is positioned at the exit of the left ventricle, where it connects to the aorta, the largest artery in the body. This valve has three cusps that open and close with each heartbeat, allowing the oxygenated blood to be pumped out of the heart and into the systemic circulation.
Lastly, we have the pulmonary valve, which is located at the exit of the right ventricle. It has three cusps that open and close to facilitate the flow of deoxygenated blood from the heart to the lungs, where it can be replenished with oxygen.
Identifying Auscultation Points
Now that we have a better understanding of the four heart valves, let’s delve into the importance of identifying the auscultation points. Auscultation, which involves listening to the sounds produced by the heart using a stethoscope, is a crucial diagnostic tool in assessing the heart’s health and detecting any abnormalities.
The auscultation points, also known as cardiac landmarks, are specific locations on the chest where the sounds of the heart are best heard. These points serve as guideposts for healthcare professionals to accurately assess the functioning of the heart valves and detect any potential issues.
The aortic area, located in the second intercostal space to the right of the sternum, is one of the key auscultation points. By placing the stethoscope in this area, healthcare providers can listen for the characteristic sounds associated with the opening and closing of the aortic valve.
The pulmonic area, situated in the second intercostal space to the left of the sternum, is another important auscultation point. Here, healthcare professionals can listen for the sounds produced by the pulmonary valve, which provide valuable insights into the functioning of the right side of the heart.
The tricuspid area, found in the lower left sternal border, is where the sounds of the tricuspid valve can be best heard. By carefully auscultating this area, healthcare providers can assess the integrity of the valve and identify any abnormalities that may affect blood flow.
Lastly, the mitral area, located in the fifth intercostal space at the midclavicular line, allows healthcare professionals to listen for the sounds produced by the mitral valve. This valve is of particular interest as it is responsible for preventing the backflow of blood from the left ventricle to the left atrium.
Accurate identification of these auscultation points and the use of appropriate techniques are essential in ensuring a precise assessment of the heart sounds. By carefully listening to the heart’s symphony, healthcare providers can gain valuable insights into the functioning of the heart valves and provide the best possible care for their patients.
Techniques for Auscultating Heart Sounds
Patient Positioning for Optimal Auscultation
The positioning of the patient during heart auscultation can significantly impact the quality of sounds heard. Positioning the patient correctly, such as in a seated or supine position, ensures the heart is appropriately aligned for optimal listening. This alignment allows healthcare professionals to accurately assess the heart sounds and detect any abnormalities that may be present.
However, patient positioning is not limited to a simple seated or supine position. In some cases, certain maneuvers can be employed to further enhance the clarity of heart sounds. For instance, asking the patient to take deep breaths can help accentuate specific heart sounds, especially those associated with valvular abnormalities. This technique allows healthcare professionals to gather more detailed information about the patient’s cardiac health.
Systematic Auscultation Approach
Adopting a systematic approach to auscultation ensures that all relevant areas are carefully assessed. Following a specific sequence, such as starting from the aortic area and moving clockwise around the chest, helps ensure consistency and accuracy in assessing various heart sounds. This systematic approach not only aids in the identification of abnormalities but also allows for the comparison of sound characteristics at different auscultation points.
During the systematic auscultation process, healthcare professionals pay close attention to the different areas of the heart, including the aortic, pulmonic, tricuspid, and mitral areas. By meticulously evaluating each of these areas, they can identify any deviations from the normal heart sounds and determine the underlying causes. This comprehensive assessment is crucial in providing accurate diagnoses and developing appropriate treatment plans for patients.
Interpreting Heart Sounds
Understanding heart sounds is a fundamental skill for healthcare professionals, especially when it comes to differentiating between normal and abnormal sounds. While normal heart sounds can vary slightly from person to person, they generally exhibit specific characteristics that can be identified through careful auscultation. These characteristics include intensity, duration, and pitch.
Normal heart sounds, often referred to as “lub-dub,” are produced by the closing of the heart valves. The first sound, known as S1, is caused by the closure of the mitral and tricuspid valves, while the second sound, S2, is produced by the closing of the aortic and pulmonary valves. These sounds are typically heard as a rhythmic, synchronized pattern, indicating the proper functioning of the heart.
Normal Heart Sounds
Familiarizing yourself with the typical features of normal heart sounds enables you to identify any deviations from the norm during auscultation. For example, the intensity of the heart sounds can vary depending on factors such as age, body size, and overall cardiovascular health. In general, a louder S1 sound may indicate a forceful closure of the mitral and tricuspid valves, while a louder S2 sound may suggest increased pressure within the aorta and pulmonary artery.
The duration of normal heart sounds is also important to consider. Normally, S1 is longer and more pronounced than S2, with a brief pause between the two sounds. However, in certain conditions, such as aortic stenosis, the duration of S2 may be prolonged, indicating a narrowing of the aortic valve.
Pitch, another characteristic of heart sounds, can provide valuable information about the condition of the heart. A higher-pitched S1 sound may indicate a stiffening of the mitral and tricuspid valves, while a higher-pitched S2 sound may suggest increased blood flow velocity within the aorta and pulmonary artery.
Abnormal Heart Sounds and What They Mean
While normal heart sounds follow a predictable pattern, abnormal heart sounds can indicate various cardiac abnormalities. These abnormal sounds, such as murmurs or additional heart sounds, can provide valuable insights into the underlying condition.
Murmurs, for example, are abnormal sounds caused by turbulent blood flow within the heart. They can be indicative of conditions such as valvular diseases, ventricular septal defects, or aortic regurgitation. The timing, loudness, pitch, and quality of the murmur can help healthcare professionals diagnose and monitor these specific cardiac disorders.
Additional heart sounds, such as S3 and S4, can also be abnormal findings. S3, commonly heard in conditions like congestive heart failure, is caused by rapid ventricular filling during the early phase of diastole. S4, on the other hand, is often associated with conditions like hypertrophic cardiomyopathy and is caused by the contraction of the atria against a stiff ventricle.
Interpreting these abnormal heart sounds requires a keen ear and a thorough understanding of cardiac physiology. By carefully analyzing the timing, loudness, pitch, and quality of these sounds, healthcare professionals can make accurate diagnoses and provide appropriate treatment for patients with cardiac abnormalities.
Common Challenges in Heart Auscultation
Overcoming Background Noise
Auscultation, the process of listening to the sounds produced by the heart using a stethoscope, can be quite challenging, especially in noisy clinical environments. The presence of background noise can interfere with the accuracy of auscultation, making it difficult for healthcare professionals to identify and interpret the subtle sounds of the heart.
To overcome background noise, healthcare professionals employ various techniques. One effective approach is to ask the patient to sit in a quiet area, away from distractions and external disturbances. This creates an environment conducive to accurate auscultation, allowing the healthcare professional to focus on the sounds of the heart without any interference.
In addition to the patient’s positioning, the correct placement of the stethoscope is crucial. Healthcare professionals are trained to position the stethoscope correctly on the patient’s chest, ensuring optimal sound transmission and minimizing the impact of external noise. This precise placement enables them to capture the heart sounds with greater clarity and accuracy.
Furthermore, advancements in technology have led to the development of auscultation devices with noise-reducing features. These devices are designed to filter out unwanted background noise, enhancing the quality of auscultation. By utilizing such devices, healthcare professionals can further minimize the impact of background noise, ensuring that the heart sounds are heard clearly and accurately.
Dealing with Patient Discomfort
While background noise poses a challenge in heart auscultation, patient discomfort or anxiety can also affect the accuracy of the procedure. It is not uncommon for patients to feel uneasy or anxious during a medical examination, especially when it involves the heart, a vital organ that holds great significance.
Healthcare professionals play a crucial role in addressing patient discomfort and ensuring a positive patient experience during heart auscultation. Creating a calming environment is essential, as it helps to alleviate the patient’s anxiety. Simple measures such as dimming the lights, playing soothing music, or providing a comfortable seating arrangement can contribute to a more relaxed atmosphere.
Moreover, effective communication between the healthcare professional and the patient is vital. Explaining the procedure in a clear and concise manner helps to demystify the process, easing the patient’s concerns. By providing information about what to expect, healthcare professionals can help patients feel more at ease and reduce any unnecessary anxiety.
Establishing a good rapport with the patient is equally important. Demonstrating empathy, actively listening to their concerns, and addressing any questions they may have can go a long way in building trust and creating a positive patient-provider relationship. Maintaining professionalism throughout the auscultation process ensures that the patient feels respected and valued, further enhancing their overall experience.
In conclusion, heart auscultation presents its own set of challenges, including background noise and patient discomfort. By employing techniques to overcome background noise and creating a calming environment for patients, healthcare professionals can enhance the accuracy of auscultation and provide a positive patient experience.
Tips for Improving Auscultation Skills
Continuous Learning and Practice
Auscultation is a skill that improves with practice and experience. Healthcare professionals should dedicate time for continuous learning and honing their auscultation skills. Regular practice with normal and abnormal heart sounds helps develop a keen ear for detecting subtle variations and enhances diagnostic accuracy.
Utilizing Auscultation Simulations and Recordings
Advancements in technology have enabled the creation of auscultation simulations and recordings. These tools allow healthcare professionals to practice their auscultation skills in a controlled environment while providing realistic heart sound representations. Utilizing such simulations and recordings can be an effective way to improve proficiency in differentiating normal and abnormal heart sounds.
Mastering the art of heart auscultation is essential for accurate diagnosis and monitoring of cardiac conditions. By understanding heart sounds, utilizing the appropriate tools, knowing the anatomy and auscultation points, applying proper techniques, and continuous practice, healthcare professionals can enhance their auscultation skills and provide optimal care to their patients.