In the field of medicine, a stethoscope is an essential tool used by healthcare professionals to listen to various sounds produced by the body, including the heart. Proper stethoscope placement is crucial to accurately assess heart sounds and detect any abnormalities. This article will provide a comprehensive guide on where to place a stethoscope to listen to heart sounds effectively.
Understanding Heart Sounds
The first step to effectively placing a stethoscope on the chest is to understand the different heart sounds that can be heard. The human heart produces two primary sounds known as S1 and S2, which correspond to the closure of the heart valves. These sounds can be best heard in specific anatomical regions of the chest.
The Basics of Heart Sounds
S1, the first heart sound, occurs when the mitral and tricuspid valves close during the contraction of the ventricles. This sound is often described as a “lub” and indicates the beginning of systole. On the other hand, S2, the second heart sound, is produced when the aortic and pulmonary valves close at the end of systole. This sound is commonly referred to as a “dub” and signifies the beginning of diastole.
The Importance of Listening to Heart Sounds
Listening to heart sounds is a fundamental part of a physical examination. By paying careful attention to these sounds, physicians can assess the overall function and health of the heart. Identifying any abnormalities in heart sounds can aid in the diagnosis and management of various cardiovascular conditions.
Furthermore, understanding the nuances of heart sounds can provide valuable insights into the underlying mechanisms of the cardiovascular system. For instance, variations in the intensity, timing, and quality of heart sounds can indicate different cardiac pathologies. A skilled healthcare professional can distinguish between normal and abnormal heart sounds, such as murmurs, gallops, or clicks, which may suggest specific conditions like valvular disorders or congenital heart defects.
Moreover, the ability to accurately interpret heart sounds can help guide treatment decisions and monitor the effectiveness of interventions. For example, changes in heart sounds after medication administration or surgical procedures can provide objective evidence of therapeutic outcomes. Additionally, serial auscultation of heart sounds over time can help track the progression or regression of certain cardiac conditions, enabling healthcare providers to adjust treatment plans accordingly.
Anatomy of the Heart and Chest
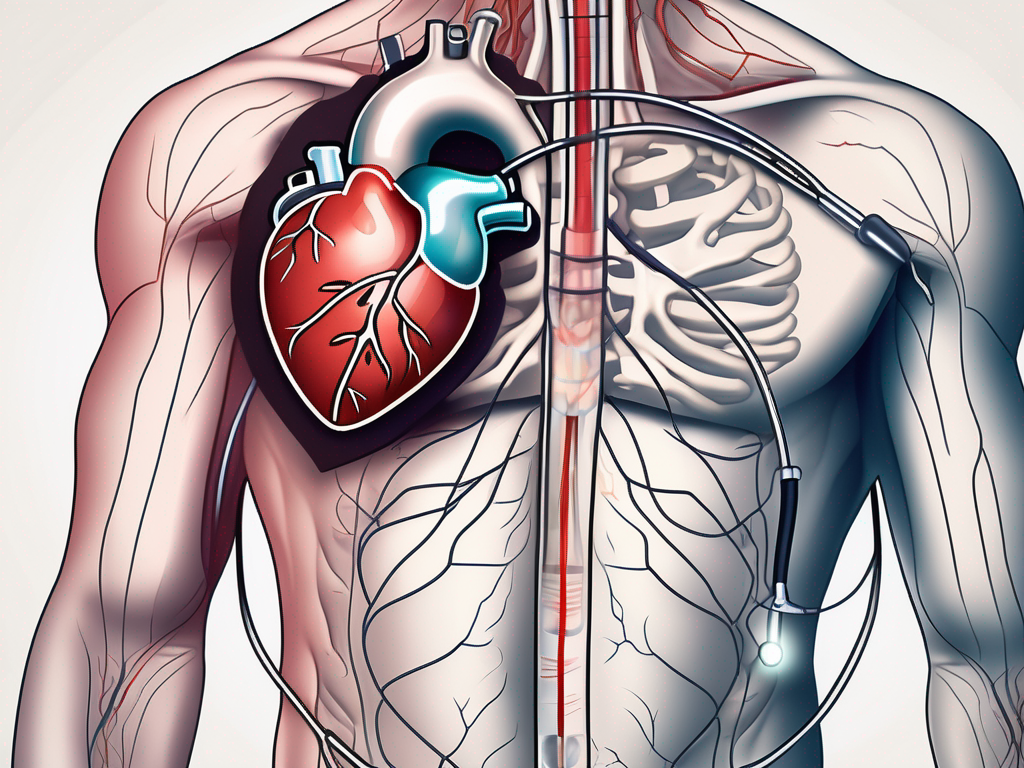
To accurately place a stethoscope on the chest, it’s essential to have a basic understanding of the anatomy of the heart and chest. The heart is a remarkable organ that plays a vital role in pumping oxygenated blood throughout the body. Located in the mediastinum, a central compartment of the chest, the heart is positioned behind the sternum (breastbone), nestled between the lungs like a precious jewel protected by its surroundings.
The heart is not just a simple pump; it is a complex structure composed of various chambers, valves, and blood vessels. Understanding the intricate design of this magnificent organ is crucial for healthcare professionals to accurately assess its health and functioning. Let’s explore some key areas that are of utmost importance when it comes to stethoscope placement.
Key Areas for Stethoscope Placement
There are four key areas on the chest where stethoscope placement is crucial for listening to heart sounds. These areas include the aortic area, pulmonic area, tricuspid area, and mitral area. Each area corresponds to a specific heart valve and provides valuable information about its functioning. By carefully positioning the stethoscope on these areas, healthcare professionals can tune into the symphony of the heart and decipher any irregularities or abnormalities that may be present.
Imagine the aortic area as the gateway to the body, where the aortic valve stands guard, regulating the flow of oxygen-rich blood into the aorta, the largest artery in the body. The pulmonic area, on the other hand, is like a gateway to the lungs, where the pulmonic valve ensures that deoxygenated blood is efficiently pumped to the lungs for oxygenation. The tricuspid area, named after the tricuspid valve, is a crucial checkpoint that allows blood to flow from the right atrium to the right ventricle. Lastly, the mitral area, also known as the apex of the heart, is where the mitral valve ensures the smooth passage of oxygenated blood from the left atrium to the left ventricle.
Understanding the Heart’s Position in the Chest
The heart is not just a mere bystander in the chest; it holds a prominent position slightly towards the left side. This unique placement allows the heart to have a more direct connection with the body’s major blood vessels, ensuring efficient blood circulation. By having a clear understanding of the heart’s location, healthcare professionals can determine the precise placement of the stethoscope and enhance their ability to detect and interpret heart sounds accurately.
So, the next time you place a stethoscope on a patient’s chest, take a moment to appreciate the intricate anatomy of the heart and chest. Remember, it is through this understanding that healthcare professionals can unlock the secrets hidden within the rhythmic beats and murmurs, providing valuable insights into the health and well-being of their patients.
The Stethoscope and Its Use
A stethoscope is an essential tool in the medical field, allowing healthcare professionals to listen to the internal sounds of the body. It consists of several components that are crucial for proper auscultation of heart sounds. Understanding these parts and how to handle them correctly is of utmost importance for achieving accurate results.
Let’s dive deeper into the different parts of a stethoscope. A typical stethoscope consists of three main components: the chest piece, tubing, and earpieces. The chest piece, also known as the head, is the part that is placed on the patient’s body to capture the sounds. It comprises a diaphragm and a bell, which are used to listen to different frequencies. The diaphragm is a flat, circular disc that is sensitive to high-frequency sounds, such as heart murmurs and lung sounds. On the other hand, the bell is a hollow, cup-shaped structure that is used to detect low-frequency sounds, like abnormal heart sounds or bruits.
Now, let’s talk about the tubing. The tubing of a stethoscope is responsible for allowing sound to travel from the chest piece to the earpieces. It is usually made of high-quality materials that minimize sound loss and interference. The length of the tubing can vary, but it is typically long enough to provide flexibility and convenience during examinations.
Lastly, we have the earpieces. These are the parts of the stethoscope that are inserted into the ears for listening. They are designed to provide a comfortable fit and a proper seal to prevent external noise from interfering with the sounds being heard. It is important to properly insert the earpieces and adjust the tension in the tubing to ensure optimal sound transmission.
Proper handling of a stethoscope is crucial for accurate auscultation. In addition to understanding the different parts, it is important to know how to handle and position the stethoscope correctly. When using a stethoscope, it is essential to hold the chest piece firmly against the patient’s skin to create an airtight seal. This ensures that the sounds are captured accurately and minimizes any external noise interference. Additionally, properly inserting the earpieces and adjusting the tension in the tubing is vital for optimal sound transmission and clarity.
The stethoscope is a remarkable tool that allows healthcare professionals to gather valuable information about a patient’s health. By understanding the different parts of a stethoscope and how to handle them correctly, healthcare professionals can ensure accurate auscultation and provide the best possible care to their patients.
Techniques for Listening to Heart Sounds
Listening to heart sounds requires proper positioning of the patient, precise stethoscope placement, and the ability to distinguish between different heart sounds. Mastering these techniques is crucial for effectively assessing the cardiac health of patients.
Positioning the Patient
Before placing the stethoscope on the chest, it is important to position the patient correctly. The patient should be in a comfortable and relaxed position, preferably lying flat on their back. This position allows for optimal access to the heart and ensures accurate placement of the stethoscope.
Additionally, it is important to consider the patient’s breathing pattern during positioning. Instructing the patient to take slow, deep breaths can help relax the chest muscles and provide a clearer sound transmission. This technique is particularly useful when assessing heart sounds in patients with respiratory conditions or those who are experiencing shortness of breath.
Optimal Stethoscope Placement
Once the patient is positioned correctly, precise stethoscope placement is key to listening to heart sounds accurately. By aligning the chest piece properly with the specified areas, healthcare professionals can focus on specific valves and detect any abnormal sounds or murmurs that may indicate underlying cardiac conditions.
It is important to note that stethoscope placement may vary depending on the patient’s age and body habitus. For example, in pediatric patients, the stethoscope may need to be positioned slightly higher on the chest to align with the location of the heart. In obese patients, it may be necessary to apply firmer pressure to ensure proper contact between the chest piece and the skin.
Identifying Different Heart Sounds
Being able to identify different heart sounds is essential in diagnosing and assessing cardiac conditions. Healthcare professionals should pay attention to the timing, intensity, pitch, and duration of the sounds. Familiarizing oneself with common heart murmurs and additional sounds will further aid in differentiating between normal and abnormal findings.
Moreover, it is important to consider the patient’s medical history and clinical presentation when interpreting heart sounds. Certain conditions, such as valvular diseases or heart failure, may present with distinct sounds that can help guide diagnosis and treatment decisions. By combining the knowledge of heart sounds with a comprehensive patient assessment, healthcare professionals can provide more accurate and individualized care.
Common Mistakes and Troubleshooting
Despite proper knowledge and technique, there are common mistakes that healthcare professionals may make when listening to heart sounds. Identifying these errors and troubleshooting poor sound quality can significantly improve the accuracy and reliability of auscultation.
Avoiding Common Errors in Stethoscope Placement
One common error is applying excess pressure or improper angulation while placing the stethoscope on the chest. This can result in distorted sounds or the unintentional muffling of important heart sounds. Being aware of these errors and avoiding them will ensure reliable auscultation.
Another important consideration is the placement of the stethoscope’s diaphragm. Placing it too close to the patient’s clothing or over bony prominences can lead to additional noise interference, making it difficult to discern the subtle nuances of heart sounds. By ensuring the diaphragm is in direct contact with the patient’s skin, healthcare professionals can minimize extraneous noise and enhance the clarity of auscultated sounds.
Troubleshooting Poor Sound Quality
Poor sound quality can significantly affect the ability to accurately assess heart sounds. Common causes include improper handling of the stethoscope, ambient noise interference, or a damaged or malfunctioning stethoscope. Troubleshooting steps, such as adjusting the earpieces, checking the tubing for obstructions, or replacing worn-out parts, can help overcome these issues.
Additionally, it is crucial to consider the environment in which auscultation is performed. High levels of ambient noise, such as bustling hospital hallways or the hum of medical equipment, can obscure heart sounds and make it challenging to detect abnormalities. Healthcare professionals should strive to create a quiet and calm environment for auscultation, ensuring optimal sound quality and accurate interpretation of heart sounds.
Maintaining Your Stethoscope for Optimal Performance
To ensure optimal performance and prolong the life of your stethoscope, proper cleaning and care are essential. But did you know that there are additional steps you can take to keep your stethoscope in top-notch condition? Let’s dive deeper into the world of stethoscope maintenance.
Cleaning and Care of Your Stethoscope
Regularly cleaning your stethoscope helps prevent the buildup of dirt, debris, and potential pathogens. Using a mild soap and water solution or disinfectant wipes, gently wipe down the chest piece, tubing, and earpieces. But here’s a pro tip: consider using a specialized cleaning solution specifically designed for stethoscopes. These solutions are formulated to effectively remove stubborn stains and maintain the integrity of the instrument.
Furthermore, proper storage in a clean and dry environment will contribute to the longevity of your stethoscope. Consider investing in a protective case or pouch to keep your stethoscope safe from dust, moisture, and accidental damage. This simple step can go a long way in preserving the performance and appearance of your trusted diagnostic tool.
When to Replace Your Stethoscope
Over time, stethoscopes may experience wear and tear or suffer damage that affects their performance. Regularly inspecting your stethoscope for cracks, loose parts, or significant deterioration is necessary. But how do you know when it’s time to replace your stethoscope?
One telltale sign is a noticeable decrease in sound quality. If you find yourself struggling to hear heart sounds clearly or if there are sudden distortions in the sound, it may be an indication that your stethoscope needs to be replaced. Additionally, if you notice any physical damage, such as a cracked chest piece or frayed tubing, it’s crucial to address the issue promptly. Ignoring these signs can lead to inaccurate auscultation and potentially compromise patient care.
Remember, maintaining your stethoscope is not just about cleanliness; it’s about ensuring accurate diagnoses and providing the best possible care for your patients. By following these additional maintenance steps and staying vigilant for signs of wear and tear, you can maximize the lifespan of your stethoscope and continue to rely on it as a trusted tool in your medical practice.