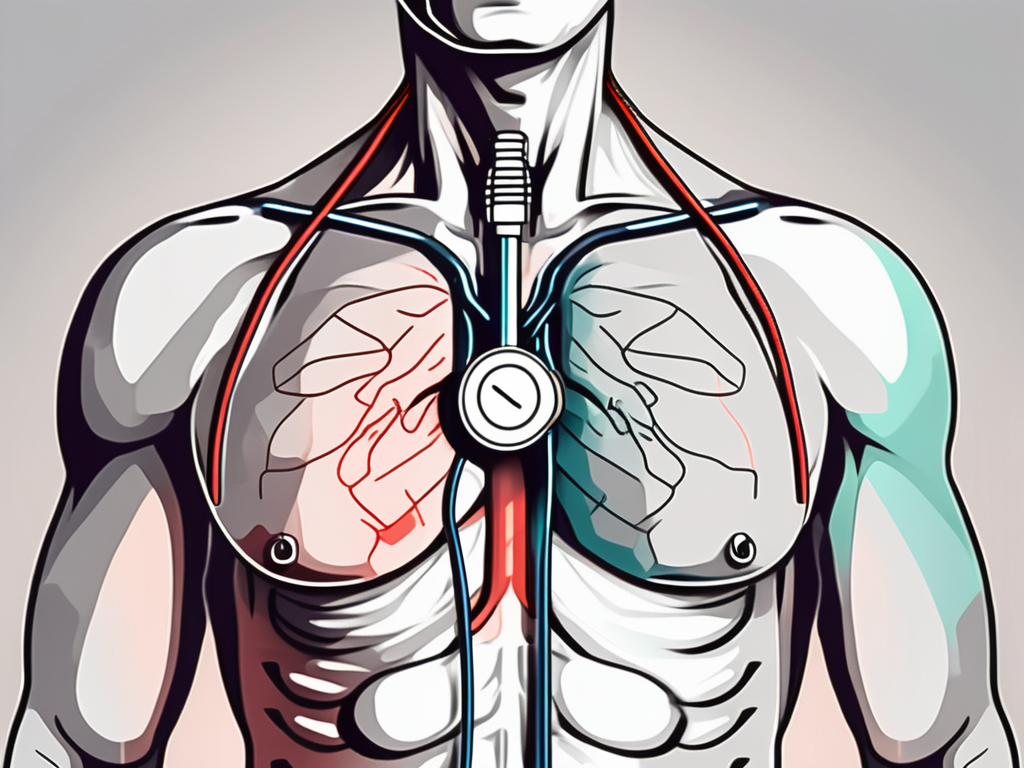
Knowing where to place the stethoscope for heart sounds is crucial for healthcare professionals and students learning to auscultate. By understanding the basics of heart sounds, the anatomy of the heart and chest, and the proper technique for listening, you can improve your ability to detect and interpret abnormal heart sounds. In this article, we will explore these topics and provide tips for clearer heart sound reception, as well as address common challenges and solutions associated with heart auscultation.
Understanding Heart Sounds
The human heart produces distinct sounds during each cardiac cycle. These sounds, commonly referred to as heart tones, provide important diagnostic information about the functioning of the heart valves and chambers. By listening to heart sounds, healthcare providers can identify any abnormalities or anomalies that may indicate underlying cardiac conditions.
The Basics of Heart Sounds
The first step in mastering the art of heart sound auscultation is understanding the different components of heart sounds. There are two main heart sounds – S1 and S2. S1 is the first heart sound and is typically described as a “lub” sound. It coincides with the closure of the mitral and tricuspid valves at the beginning of systole. S2, on the other hand, is the second heart sound and is often described as a “dub” sound. It occurs when the aortic and pulmonary valves close at the beginning of diastole.
Each of these heart sounds can be further divided into specific components known as murmurs. Murmurs are abnormal or additional sounds heard during auscultation, which may indicate valve abnormalities, heart defects, or other cardiac conditions.
The Importance of Listening to Heart Sounds
Accurate interpretation of heart sounds is crucial for diagnosing and monitoring cardiac conditions. By listening carefully to the heart sounds, healthcare providers can detect abnormalities such as heart murmurs, arrhythmias, and valve disorders. This information helps in determining the appropriate course of treatment and enhancing patient outcomes.
Furthermore, the skill of auscultating heart sounds is not limited to healthcare providers alone. Patients with certain cardiac conditions can also benefit from learning how to listen to their own heart sounds. This can empower them to detect any changes or abnormalities in their heart rhythm, and seek timely medical attention if necessary.
Moreover, advancements in technology have led to the development of electronic stethoscopes equipped with digital sound filters and amplifiers. These devices enable healthcare providers to enhance the clarity and quality of heart sounds, making it easier to detect subtle abnormalities that may have been missed with traditional stethoscopes.
Anatomy of the Heart and Chest
In order to auscultate heart sounds effectively, one must have a sound understanding of the heart’s anatomy and the key areas for listening to heart sounds. The heart is located within the chest cavity and is primarily composed of four chambers – the left and right atria and ventricles.
The left atrium receives oxygenated blood from the lungs through the pulmonary veins, while the right atrium receives deoxygenated blood from the body through the superior and inferior vena cava. The atria contract simultaneously, pushing the blood into the ventricles.
The ventricles, on the other hand, are responsible for pumping the blood out of the heart. The left ventricle pumps oxygenated blood to the rest of the body through the aorta, while the right ventricle pumps deoxygenated blood to the lungs through the pulmonary artery.
Key Areas for Listening to Heart Sounds
When placing the stethoscope for heart sound auscultation, it is important to target specific areas known as auscultatory areas. These areas correspond to specific valves and provide the best auditory access to the underlying cardiac structures. The auscultatory areas include the mitral, tricuspid, aortic, and pulmonary areas, which are located at various points on the chest and back.
The mitral area, also known as the apex of the heart, is located at the fifth intercostal space in the midclavicular line. This area is best for listening to the mitral valve, which separates the left atrium from the left ventricle. The tricuspid area, located at the fourth intercostal space along the left sternal border, allows for the assessment of the tricuspid valve between the right atrium and right ventricle.
The aortic area, found at the second intercostal space along the right sternal border, is ideal for detecting abnormalities in the aortic valve. Lastly, the pulmonary area, situated at the second intercostal space along the left sternal border, provides access to the pulmonary valve between the right ventricle and the pulmonary artery.
Understanding the Heart’s Structure
The heart is composed of specialized muscle tissue that contracts rhythmically to pump blood throughout the body. It is essential to have a basic understanding of the heart’s structure in order to interpret heart sounds accurately. Familiarize yourself with the location and function of the heart valves and chambers to enhance your ability to detect abnormalities during auscultation.
The heart valves, including the mitral, tricuspid, aortic, and pulmonary valves, ensure the unidirectional flow of blood through the heart. The mitral and tricuspid valves are atrioventricular valves that prevent the backflow of blood from the ventricles to the atria during ventricular contraction. The aortic and pulmonary valves, on the other hand, are semilunar valves that prevent the backflow of blood from the arteries to the ventricles during relaxation.
By understanding the intricate structure of the heart and the role of each component, healthcare professionals can effectively assess heart sounds and identify any potential abnormalities that may require further investigation or treatment.
The Stethoscope and Its Role
The stethoscope is an essential tool for auscultation and plays a vital role in accurately detecting and interpreting heart sounds. A stethoscope consists of a chest piece, tubing, and earpieces. The chest piece contains a diaphragm and a bell, which are used for listening to different frequencies of sound.
How a Stethoscope Works
The diaphragm of the stethoscope is used for high-frequency sounds, such as S1 and S2. It is best suited for detecting normal heart sounds. The bell, on the other hand, is used for low-frequency sounds, such as heart murmurs and abnormal heart sounds. Understanding how the different parts of the stethoscope work together is crucial for accurate auscultation.
Choosing the Right Stethoscope
When selecting a stethoscope, it is important to consider factors such as the quality of sound transmission, comfort, and durability. There are various types of stethoscopes available, including acoustic and electronic options. By choosing a stethoscope that meets your specific needs, you can enhance the accuracy and efficiency of heart sound auscultation.
Aside from the technical aspects, the stethoscope holds a symbolic significance in the medical field. It is a powerful emblem of the doctor-patient relationship, representing trust, expertise, and care. The simple act of placing the stethoscope on a patient’s chest creates a connection between the healthcare provider and the individual seeking medical attention. It is a tangible reminder that the doctor is there to listen, both literally and figuratively, to the patient’s concerns and symptoms.
Furthermore, the stethoscope has a rich history that dates back to the early 19th century. It was invented by René Laennec, a French physician, who sought a more effective way to listen to the sounds of the heart and lungs. Laennec’s invention revolutionized the field of medicine, allowing doctors to diagnose and treat various cardiovascular and respiratory conditions with greater accuracy. Today, the stethoscope remains an indispensable tool in the medical profession, serving as a constant reminder of the advancements made in healthcare over the years.
Techniques for Listening to Heart Sounds
Listening to heart sounds requires a systematic approach and proper technique. By following these guidelines, you can improve your ability to detect and interpret abnormal heart sounds.
When positioning the stethoscope correctly, it is essential to consider the anatomical landmarks. The aortic valve is best heard at the second intercostal space, right sternal border. The pulmonic valve is best heard at the second intercostal space, left sternal border. The tricuspid valve is best heard at the fourth intercostal space, left sternal border. Lastly, the mitral valve is best heard at the fifth intercostal space, midclavicular line. By knowing these specific locations, you can ensure accurate placement of the stethoscope and enhance your ability to detect subtle abnormalities.
Positioning the Stethoscope Correctly
To effectively auscultate heart sounds, it is important to position the stethoscope correctly. Place the diaphragm or bell of the stethoscope directly over the target area, ensuring a tight seal for optimal sound transmission. Take your time to ensure proper placement before starting the auscultation.
Moreover, it is crucial to consider the patient’s body position during auscultation. The ideal position for listening to heart sounds is with the patient sitting upright, leaning slightly forward. This position helps to bring the heart closer to the chest wall, making it easier to hear the sounds. However, in certain cases where the patient is unable to sit up, such as in the intensive care unit, you can adjust the bed to a semi-Fowler’s position to achieve a similar effect.
Identifying Normal and Abnormal Heart Sounds
Developing the skill to differentiate between normal and abnormal heart sounds is crucial for accurate diagnosis. Familiarize yourself with the characteristics of normal heart sounds and the different types of murmurs. This will enable you to identify potential abnormalities and refer patients for further evaluation when necessary.
One way to enhance your ability to identify abnormal heart sounds is by familiarizing yourself with the concept of heart sound splitting. This occurs when the closure of the aortic and pulmonic valves is not synchronized, resulting in a split sound during auscultation. Understanding the causes and implications of heart sound splitting can provide valuable insights into a patient’s cardiovascular health.
Furthermore, it is important to consider the patient’s clinical history and physical examination findings when interpreting heart sounds. Certain conditions, such as valvular heart disease or myocardial infarction, can manifest with specific auscultatory findings. By integrating these findings into your assessment, you can improve your diagnostic accuracy and provide optimal care for your patients.
Tips for Clearer Heart Sound Reception
Obtaining clear heart sound reception is essential for accurate auscultation. By following these tips, you can improve the quality of heart sound reception and minimize potential obstacles.
Patient Positioning and Preparation
Proper patient positioning plays a significant role in achieving clearer heart sound reception. Ensure that the patient is in a comfortable position, lying flat if possible. This position helps to optimize the transmission of heart sounds and reduces the chances of any external factors interfering with the auscultation process. Additionally, it is important to eliminate any clothing or obstacles that may interfere with sound transmission, such as thick clothing or jewelry. These items can create unnecessary noise and hinder the accurate detection of heart sounds.
Furthermore, it is crucial to prepare the patient before starting the auscultation. Explain the procedure to them, reassuring them that it is a painless and non-invasive process. This will help to alleviate any anxiety or tension that the patient may have, ensuring they are relaxed and cooperative during the examination. Remember, a calm and comfortable patient is more likely to provide clearer heart sounds, leading to a more accurate diagnosis.
Reducing Background Noise
Noise interference can compromise the clarity of heart sounds, making it difficult to distinguish between different cardiac events. To minimize background noise in the auscultation environment, it is essential to create a quiet and controlled setting. Choose a room that is free from excessive noise, such as traffic or loud conversations. If such a room is not available, consider using noise-canceling techniques to reduce external disturbances.
One effective technique is to ask the patient to breathe quietly and avoid unnecessary movement during the auscultation. This helps to reduce any additional noise that may be generated, allowing you to focus solely on the heart sounds. Additionally, using a stethoscope with good noise-canceling capabilities can further enhance the clarity of the heart sounds by minimizing external noise interference.
Remember, the ability to accurately detect and interpret heart sounds is crucial for making informed clinical decisions. By implementing these tips, you can optimize the quality of heart sound reception, leading to more accurate diagnoses and improved patient outcomes.
Common Challenges and Solutions
Heart sound auscultation can present challenges that may affect the accuracy of diagnosis. By being aware of these challenges and implementing appropriate solutions, you can improve your auscultation skills and overcome these obstacles.
Dealing with Difficulties in Hearing Heart Sounds
In certain situations, external factors or patient-specific characteristics may make it challenging to hear heart sounds clearly. Learn strategies to overcome these difficulties, such as adjusting the pressure of the stethoscope or changing the patient’s position to optimize sound transmission.
Troubleshooting Stethoscope Issues
Stethoscope malfunctions can negatively impact the accuracy of heart sound auscultation. Familiarize yourself with common stethoscope issues and troubleshooting techniques, such as ensuring proper tube alignment and regular maintenance, to prevent potential problems.
Another challenge that healthcare professionals may encounter during heart sound auscultation is the presence of background noise. In a busy hospital setting, it can be difficult to isolate and focus on the subtle sounds of the heart. To address this issue, consider finding a quiet area for auscultation or using noise-cancelling headphones to minimize distractions.
Furthermore, patient factors, such as obesity or excessive chest hair, can pose challenges in obtaining clear heart sounds. In these cases, it may be helpful to use additional techniques to enhance sound transmission. For example, applying a thin layer of ultrasound gel between the stethoscope and the patient’s skin can improve the conduction of sound waves, allowing for better detection of heart murmurs or abnormalities.
Conclusion: Mastering the Art of Heart Sound Auscultation
Auscultating heart sounds is a fundamental skill for healthcare providers. By understanding the basics of heart sounds, the anatomy of the heart and chest, and utilizing proper techniques, you can improve your ability to accurately detect and interpret abnormal heart sounds. Remember to choose the right stethoscope and position it correctly to ensure clear heart sound reception. With practice and knowledge, you can master the art of heart sound auscultation and provide the best possible care for your patients.